NIPT: Non-Invasive, Informed, and a Key to Reproductive Autonomy
Women who chose NIPT often reported that they were very satisfied of their choice and felt confident and well-informed. There is however still a need to examine how women get access and are able to comprehend the information on NIPT as well as how they access counseling prior to birth in order for them to take informed and responsible choices.
Non Invasive Prenatal Testing and Reproductive Planning
When NIPT grows more readily available and more widely available, it’s important for clinicians to be well-versed on how to provide accurate and clear details about the test. Studies have found that women desire and require access to information of high-quality on NIPT to make autonomous decisions. The information is essential to encouraging reproductive autonomy which is among the key concepts of informed decision-making.
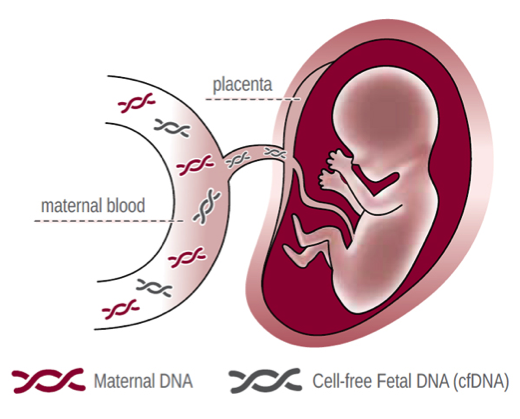
It is a non-invasive test that makes use of the mother’s blood in order to identify indications of chromosomal anomalies on her infant. It will reveal Edward syndrome (duplication of the 2 chromosomes, X and Y), Patau syndrome (trisomy 13) or Down syndrome (trisomy 21). If a positive result is detected, a more invasive diagnostic test, such as amniocentesis or CVS is likely to confirm the finding.
Genetic Abnormality Detection in Reproductive Planning
NIPT is not associated with any risks to pregnant women, unlike other diagnostic tests, such as amniocentesis or chronic villus sampling (CVS). It employs cells-free DNA (cfDNA) taken from the blood of the mother to find aneuploidy using the chromosome count.
This test is an ideal choice for pregnancies with high risks and those with contraindications to the invasive procedure. However, the results may not be 100% accurate.
It was suggested that If NIPT is made routine and is offered as a normal pregnant test, this might compromise reproductive autonomy, increasing the likelihood of stigmatisation for people who have disabilities, and result in unintentional use of these tests. To stop this from happening specialists stressed that counsellors is not limited to explaining the technical details of NIPT, and clear up misconceptions regarding disability and testing as well as explore the women’s perceptions to NIPT, and the intention to raise children with disabilities.
Role of NIPT in Family Planning
The NIPT screening test is, and not a diagnostic instrument. If the results of a woman’s NIPT suggest a risky presence of the presence of an anomaly, her OB/GYN or midwife might recommend testing for genetic disorders that require more effort, such as chorionic villus samples (CVS) as well as amniocentesis. This involves drawing a little amount of placenta from the uterus, and come with a risk of miscarriage.
A few respondents believed that the screening for pre-tests in NIPT needs to be improved: it is important to women having access to information about their condition, however, they might not make informed choices based on the information offered. In addition, expanding the NIPT’s scope by incorporating more issues will require more out-of-pocket expenses, that could be disproportionately affecting women with low incomes.
Respondents also feared they NIPT xet nghiem nipt o ha noi might lead to the birth of more children who have Down syndromes, Edwards’ syndrome and Patau’s syndrome. They feared that this would raise the cost of care for children with these conditions, and also their demand for support and special education assistance.
Ethical Considerations in Prenatal Decision Making
Several ethical issues arise with NIPT offered to women in public health systems. In our study, participants typically opposed the idea of a policy which would prioritise access to NIPT with respect to certain medical conditions. They argued that the determination of what fertility outcomes are “worth living’ should be left to the individual discretion of couples and not be based on priori assessments of how serious each condition is.
The blood of a pregnant woman is a reservoir of DNA and sperm of her fetus. This is known as fetal cell-free DNA (cffDNA). A NIPT test analyzes this CffDNA in order to identify the presence or absence of genetic issues like Down syndrome and other chromosomal conditions. The participants were worried about the possibility that testing could result in a feeling of pressure to test due to fears about the industry’s influence in the informational material and incentives for health providers to advocate for testing with NIPT.
Access and Cost of NIPT in Reproductive Planning
The NIPT test is more expensive than other tests for screening and isn’t covered by Medicare or health insurance plans for private individuals in Australia. It is suggested that women discuss their options with an expert in genetic counseling before making a decision whether or not to undergo the test.
The DNA for a developing pregnancy is circulated through the bloodstream of the mother and researchers can identify it with a simple laboratory test. This is known as cell-free fetal DNA (cffDNA). NIPT is only required for a tiny mother’s blood sample, it does not put the woman at any chance.
Women’s qualitative interviews conducted by Van der Meij and colleagues reveal that the majority of women who took NIPT did so because it offered reassurance and further information about their pregnancy. But, many of the women who chose not to take the test were doing so due to the fact that they did not feel a moral obligation to undergo it.